Could the pain and discomfort of pelvic inflammatory disease (PID) be treated effectively without antibiotics or surgery? As a serious gynecological condition affecting the female reproductive organs, PID requires prompt and appropriate treatment to prevent long-term, potentially devastating complications like infertility and chronic pelvic pain. In this comprehensive guide, we’ll explore the various treatment options for PID, from the role of antibiotics to the necessity of surgical intervention, as well as strategies for prevention and managing the aftermath of this complex condition.
Key Takeaways
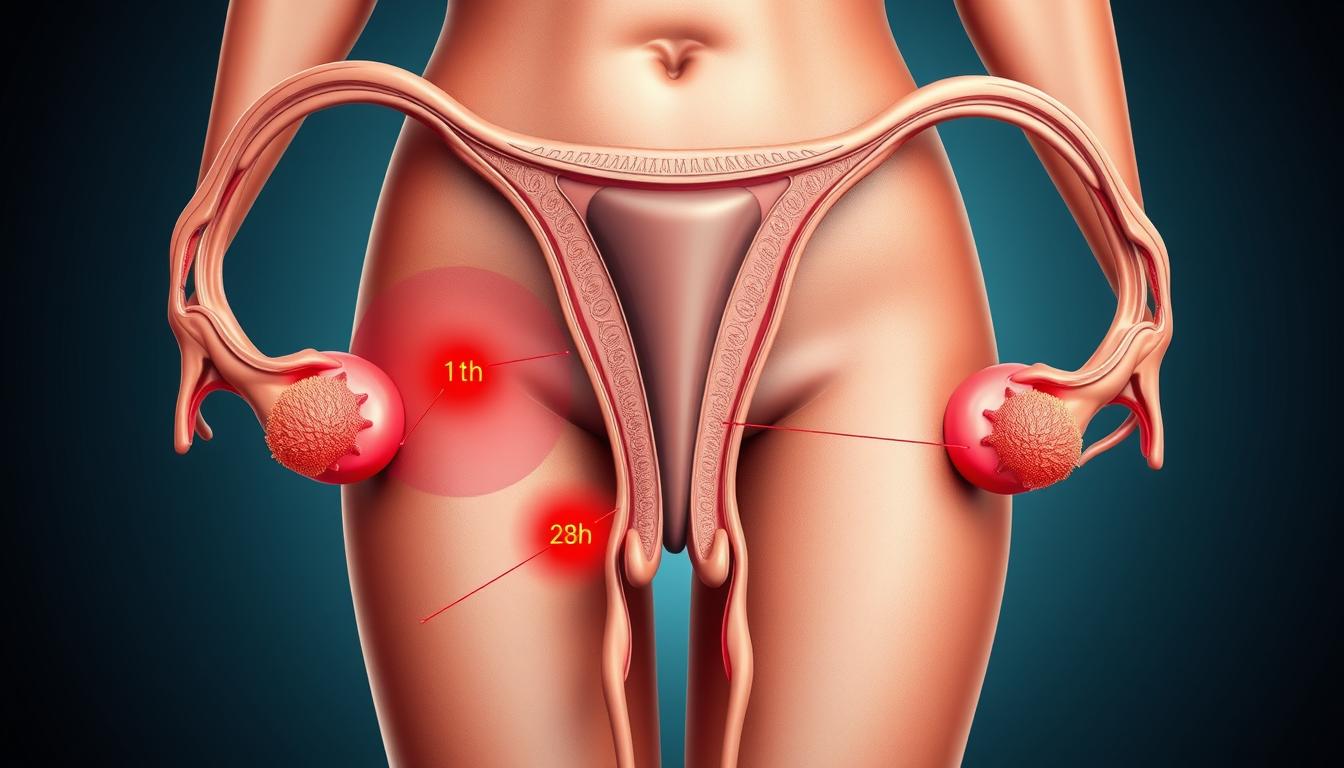
- Pelvic inflammatory disease is a serious infection and inflammation of the female upper reproductive organs, including the uterus, fallopian tubes, and ovaries.
- Prompt treatment is crucial to prevent long-term complications like infertility and chronic pelvic pain.
- Antibiotic therapy is the primary treatment approach, with both inpatient and outpatient regimens available.
- Surgical intervention, though rare, may be necessary in certain cases, such as when abscesses or uncertain diagnoses are present.
- Prevention through safe sex practices and early treatment of sexually transmitted infections can help reduce the risk of developing pelvic inflammatory disease.
What is Pelvic Inflammatory Disease?
Causes and Risk Factors
Pelvic inflammatory disease (PID) is typically caused by an ascending infection from the lower genital tract. The majority of PID cases, around 85%, are linked to sexually transmitted infections (STIs) like Neisseria gonorrhoeae or Chlamydia trachomatis. Other bacteria associated with bacterial vaginosis can also contribute to PID.
Risk factors for developing PID include having multiple sexual partners, a history of PID, and using an intrauterine device (IUD). Prompt diagnosis and treatment are crucial to prevent long-term reproductive complications.
- Many types of bacteria can cause PID, with gonorrhea or chlamydia infections being the most common.
- Factors that increase the risk of PID include being sexually active and younger than 25 years old, having multiple sexual partners, and engaging in sex without a condom.
- Douching regularly can upset the balance of good versus harmful bacteria in the vagina and might mask symptoms of PID.
- A small increased risk of PID exists after the insertion of an intrauterine device (IUD), especially in the first three weeks after insertion.
“Delaying treatment for PID dramatically increases the risk of infertility.”
Approximately 2.5 million people assigned female at birth in the U.S. will have Pelvic Inflammatory Disease (PID) at some point in their lives. Prompt treatment is essential to avoid serious complications such as infertility and chronic pelvic pain.
Diagnosis of Pelvic Inflammatory Disease
Diagnosing pelvic inflammatory disease (PID) typically involves a combination of clinical assessment and diagnostic testing. The primary focus is on identifying the characteristic signs and symptoms associated with this condition.
Signs and Symptoms
The most common signs and symptoms of PID include:
- Pelvic pain: Women with PID often experience lower abdominal or pelvic pain, which can range from mild to severe.
- Vaginal discharge: Abnormal vaginal discharge, sometimes with an unpleasant odor, is a frequent symptom of PID.
- Cervical motion tenderness: Healthcare providers may detect cervical motion tenderness during a pelvic examination.
Other common signs and symptoms include fever, abnormal bleeding, and painful intercourse.
Diagnostic Tests
While the diagnosis of PID is primarily clinical, healthcare providers may order additional diagnostic tests to support the diagnosis and rule out other conditions. These tests may include:
- Nucleic acid amplification tests (NAATs) for sexually transmitted infections, such as chlamydia and gonorrhea.
- Pregnancy tests to exclude ectopic pregnancy.
- Imaging studies, such as transvaginal ultrasound, to evaluate the pelvic organs and detect any abscesses or other complications.
It is important to note that treatment for PID should not be delayed while waiting for the results of these diagnostic tests. Prompt antibiotic therapy is crucial to prevent long-term complications.
| Diagnostic Test | Purpose |
|---|---|
| Nucleic Acid Amplification Tests (NAATs) | Detect the presence of sexually transmitted infections, such as chlamydia and gonorrhea, which are common causes of PID. |
| Pregnancy Tests | Rule out the possibility of an ectopic pregnancy, which can be a serious complication of PID. |
| Imaging Studies (e.g., Transvaginal Ultrasound) | Evaluate the pelvic organs and detect any abscesses or other complications associated with PID. |
“The diagnosis of PID is primarily clinical, based on a woman’s symptoms and a pelvic exam.”
pelvic inflammatory disease treatment
Pelvic inflammatory disease (PID) is a serious condition that requires prompt and effective treatment to prevent long-term complications such as infertility and chronic pelvic pain. The treatment for PID typically involves a combination of antibiotic to cover the most common causative pathogens, including Chlamydia trachomatis, Neisseria gonorrhoeae, Mycoplasma genitalium, and various anaerobic organisms.
In severe cases, or when the patient is pregnant, inpatient treatment with intravenous antibiotics may be warranted. This approach is also recommended when there is a failure of outpatient therapy or if surgical intervention is needed. For milder cases, outpatient oral antibiotic regimens are often appropriate. Regardless of the treatment approach, the timely initiation of treatment is crucial to minimize the risk of long-term complications.
According to a study, the prevalence of laboratory-confirmed gonorrhea and/or chlamydia rates in clinically diagnosed pelvic inflammatory disease and cervicitis is 30% (Burnett et al., 2012). Additionally, studies have revealed a statistical association between pelvic inflammatory disease and Trichomonas vaginalis infection (Cherpes et al., 2006).
“The prevalence of fluoroquinolone resistance in Neisseria gonorrhoeae is nearly 100% in some regions, rendering these agents no longer recommended for treating Neisseria gonorrhoeae infections.”
Considerations for Antibiotic Therapy
The choice of antibiotic therapy for PID should take into account the local prevalence of antibiotic resistance, as well as the patient’s clinical presentation and any contraindications. In regions with high rates of fluoroquinolone resistance in Neisseria gonorrhoeae, these agents are no longer recommended for the treatment of PID.
- Inpatient treatment regimens may involve the use of intravenous antibiotics, such as cefoxitin or ceftriaxone, in combination with doxycycline.
- Outpatient treatment options typically include a combination of oral antibiotics, such as doxycycline and metronidazole or clindamycin.
Regardless of the treatment approach, it is essential to ensure that the patient’s sexual partners are also tested and treated to prevent the recurrence or spread of the infection.
Antibiotic Therapy for PID
Effective antibiotic treatment is crucial in managing pelvic inflammatory disease (PID). The recommended approach typically involves a combination of intravenous and oral antibiotics to target the various pathogens responsible for this condition.
Inpatient Treatment Regimens
For patients requiring hospitalization, intravenous antibiotic therapy is often the initial course of action. Common regimens include a combination of cefotetan plus doxycycline or cefoxitin plus doxycycline. These intravenous antibiotics work to quickly address the infection and provide symptom relief.
Outpatient Treatment Options
For milder cases of PID, outpatient treatment with oral antibiotics may be appropriate. The Centers for Disease Control and Prevention (CDC) recommends regimens such as doxycycline plus ceftriaxone or cefoxitin with probenecid. In some cases, metronidazole may be added if there are concerns about anaerobic infections.
Regardless of the specific antibiotic regimen, it is crucial that patients complete the full course of treatment, even if their symptoms improve quickly. Discontinuing antibiotics prematurely can lead to treatment failure and the potential for antibiotic resistance.
| Inpatient Treatment | Outpatient Treatment |
|---|---|
| Cefotetan plus doxycycline | Doxycycline plus ceftriaxone |
| Cefoxitin plus doxycycline | Cefoxitin with probenecid |
Completing the full course of antibiotics, even if symptoms improve quickly, is essential for successful treatment and to prevent the development of antibiotic resistance.
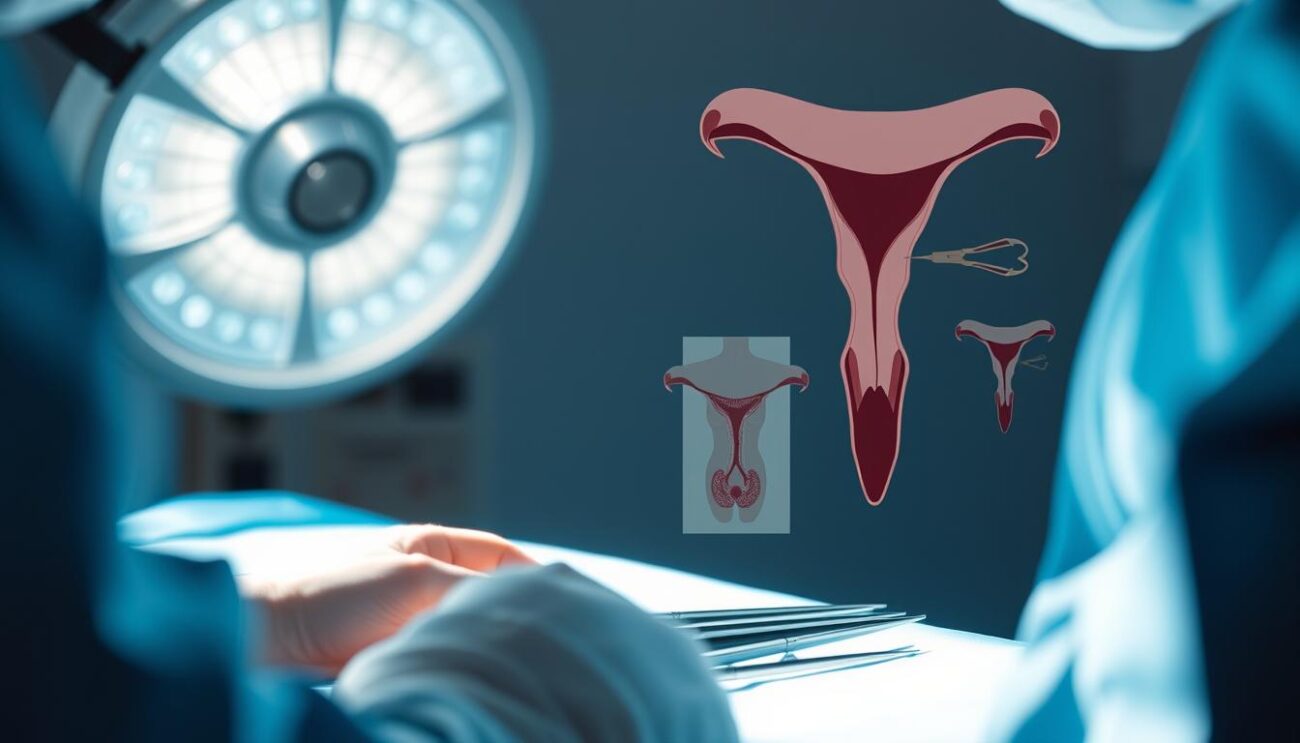
Surgical Intervention for PID
When it comes to pelvic inflammatory disease (PID), surgery is typically a last resort. However, in certain cases, surgical treatment may be necessary to address the underlying issues and prevent severe complications. The surgical treatment for PID is primarily indicated for cases where the condition does not respond to antibiotic therapy or when there is a risk of complications like pelvic abscess or tubo-ovarian abscess.
One of the primary reasons for surgical intervention in PID is the presence of a pelvic or tubo-ovarian abscess that threatens to rupture. In such scenarios, surgical drainage may be required to prevent the spread of infection and potentially life-threatening consequences. Laparoscopy, a minimally invasive surgical procedure, can also be employed to confirm the diagnosis, particularly when the clinical presentation is atypical or the patient has not shown improvement with antibiotics.
- Surgical treatment for PID may be necessary in cases of:
- Pelvic abscess
- Tubo-ovarian abscess
- Acute spreading peritonitis
- Intestinal obstruction
- Ruptured tubo-ovarian abscess
- Laparoscopic procedures can be used to:
- Confirm the diagnosis
- Address external adhesions in cases of tubal blockage
- Drain pelvic or tubo-ovarian abscesses
It is important to note that surgical intervention for PID is a rare occurrence, as the majority of cases can be effectively managed with a combination of antibiotic therapy and conservative treatment. However, in severe or complicated cases, surgical treatment may be necessary to prevent further complications and ensure the best possible outcome for the patient.
Preventing Pelvic Inflammatory Disease
Safe Sex Practices
Preventing pelvic inflammatory disease (PID) starts with practicing safe sex. This includes consistently using condoms during sexual activity and limiting the number of sexual partners. Regular testing and prompt treatment for any sexually transmitted infections (STIs) can also help reduce the risk of developing PID.
Consistent condom use is crucial, as it helps prevent the transmission of bacteria and viruses that can lead to PID. Additionally, limiting the number of sexual partners decreases the likelihood of contracting an STI that could potentially cause PID.
Regular screening for chlamydia and gonorrhea, the two most common bacterial causes of PID, is also essential. Early detection and treatment of these infections can prevent the development of PID, as well as its associated complications, such as infertility and ectopic pregnancy.
“Approximately 1 million women in the United States experience an episode of symptomatic pelvic inflammatory disease (PID) each year.”
By practicing safe sex, getting tested for STIs, and seeking prompt treatment when necessary, women can significantly reduce their risk of developing pelvic inflammatory disease and its potentially serious consequences.
Complications of Untreated PID
Pelvic Inflammatory Disease (PID) is a serious condition that, if left untreated, can lead to various long-term complications. Two of the most concerning issues associated with untreated PID are infertility risks and chronic pelvic pain.
Infertility Risks
PID can cause significant damage to the fallopian tubes, which play a crucial role in fertility. Scarring or abscesses in the tubes can block or impair their function, making it difficult for eggs to pass into the uterus. Research shows that individuals successfully treated for PID have the same pregnancy rates as the general population. However, repeated episodes of PID are linked to an increased risk of infertility. In some cases, surgical intervention may be necessary to address the damage, but assisted conception techniques like IVF can also be considered for those unable to conceive naturally.
Chronic Pelvic Pain
Untreated PID can lead to the formation of scar tissue between internal organs, causing ongoing pelvic pain and potentially increasing the risk of ectopic pregnancy. In fact, up to one-third of women with a history of PID may experience chronic pelvic pain, which can significantly impact their quality of life and lead to further problems such as depression and insomnia. Prompt and effective treatment of PID is crucial to minimize these long-term complications.
“Untreated PID can result in chronic infection, possibly causing infertility in women.”
PID in Pregnancy
Pelvic Inflammatory Disease (PID) during pregnancy is a serious condition that requires prompt medical attention. Pregnant women with suspected PID often require hospitalization for intravenous antibiotic therapy. This is because PID in pregnancy carries a higher risk of severe complications, such as preterm delivery and adverse maternal/fetal outcomes.
Prompt treatment is crucial to protect the health of both the mother and the developing fetus. Clinicians must be vigilant in recognizing the signs and symptoms of PID in pregnant women, which may include pelvic pain, fever, vaginal discharge, and irregular bleeding.
Diagnostic tests, such as urine pregnancy tests, STI screenings, and pelvic imaging, are important to confirm the diagnosis and rule out other potential causes of the symptoms. Once PID is diagnosed, the treatment plan will focus on using antibiotics that are safe for the fetus, such as ceftriaxone, cefoxitin, and erythromycin.
Hospitalization is often necessary for pregnant women with PID, as it allows for close monitoring and the administration of intravenous antibiotics. This helps to prevent the spread of infection and minimize the risk of serious complications. After treatment, close follow-up care and monitoring are essential to ensure a successful recovery and a healthy pregnancy outcome.
| Key Statistics on PID in Pregnancy | Value |
|---|---|
| Percentage of sexually experienced women who have had PID | 4.4% |
| Estimated number of women in the U.S. diagnosed with PID each year | 800,000 |
| Chance of infertility for women who have had PID | 20% |
| Risk of ectopic pregnancy for women who have had PID | 9% |
| Chance of developing chronic pelvic pain after PID | 18% |
Preventing PID in pregnancy is crucial, and this can be achieved through safe sex practices, regular STI screenings, and prompt treatment of any infections. By working closely with their healthcare providers, pregnant women can reduce their risk of developing PID and ensure a healthy pregnancy and delivery.
Follow-up Care and Monitoring
After receiving treatment for pelvic inflammatory disease (PID), close follow-up care is crucial to monitor for symptom resolution and prevent recurrent infections. Patients should return for a follow-up visit within 3 days of starting treatment to ensure the antibiotics are effectively addressing the infection.
Women with a history of PID face an increased risk of recurrent infections, which can lead to further reproductive damage. Ongoing management of any chronic pelvic pain or other complications may also be necessary as part of the follow-up process.
Importance of Regular Checkups
Regular checkups are essential for women who have experienced PID. The follow-up visits allow healthcare providers to:
- Confirm the resolution of symptoms
- Monitor for any recurrence of the infection
- Assess the need for continued treatment or management of complications
Prompt treatment of PID is crucial to prevent permanent damage to the female reproductive organs. By staying vigilant with follow-up care, women can reduce their chances of long-term complications, such as infertility and ectopic pregnancy.
Addressing Recurrent PID and Chronic Pelvic Pain
Women with a history of recurrent PID or chronic pelvic pain may require more intensive follow-up and management. Healthcare providers may recommend:
- Ongoing antibiotic therapy to prevent future infections
- Pelvic imaging, such as ultrasound or laparoscopy, to assess the extent of reproductive damage
- Referral to a specialist for the management of chronic pelvic pain
By addressing these persistent issues, healthcare providers can help women with a history of PID maintain their reproductive health and quality of life.
| Statistic | Value |
|---|---|
| Annual PID cases in the US | Over 750,000 |
| PID-related infertility rate | Around 15% |
| PID-related ectopic pregnancy rate | Up to 15% |
These statistics underscore the importance of diligent follow-up care and monitoring for women who have experienced PID. By staying proactive, healthcare providers and patients can work together to mitigate the long-term consequences of this serious reproductive health condition.
Conclusion
Pelvic inflammatory disease (PID) is a serious and complex infection that requires prompt diagnosis and comprehensive treatment to prevent long-term complications. The pelvic inflammatory disease summary highlights the critical importance of addressing this condition, as it affects nearly 1 million women annually in the United States, with a significant burden on adolescents.
The key takeaways from this discussion on PID include the need for early detection, appropriate antibiotic therapy, and close follow-up to monitor for resolution of symptoms and address any long-term consequences. Practitioners must remain vigilant in recognizing the diverse range of causative agents and the potential for asymptomatic infections, which can pose a significant risk for infertility and chronic pelvic pain.
Ultimately, a comprehensive approach to PID management, encompassing prevention, diagnosis, treatment, and long-term care, is essential to safeguard the reproductive health and well-being of women across all age groups. By addressing this critical gynecological issue, healthcare providers can empower patients, reduce the burden of this condition, and promote better overall outcomes for those affected by pelvic inflammatory disease.