Do you know the main differences between type 1 and type 2 diabetes? Both conditions involve high blood sugar, but they have key differences in causes, onset, and treatment. Knowing these differences is vital for managing your health and avoiding diabetes complications.
Type 1 diabetes is an autoimmune disease. It happens when the body attacks and destroys insulin-making cells in the pancreas. This means the body can’t make insulin, a key hormone for blood sugar control. Type 2 diabetes, however, is about insulin resistance. The body can’t use insulin well, leading to high blood sugar levels.
The way these diabetes types start is different too. Type 1 diabetes often starts quickly, usually in kids, teens, or young adults. Symptoms include a lot of thirst, needing to pee a lot, and losing weight without trying. Type 2 diabetes starts more slowly. Its symptoms might be milder, making it harder to catch early.
Managing type 1 and type 2 diabetes is also different. Type 1 needs lifelong insulin and careful blood sugar checks. Type 2 can sometimes be managed with diet, exercise, and sometimes pills or insulin.
Key Takeaways
- Type 1 diabetes is an autoimmune disorder, while type 2 diabetes is characterized by insulin resistance.
- Type 1 diabetes often develops quickly in childhood or young adulthood, while type 2 diabetes has a more gradual onset.
- Management of type 1 diabetes requires insulin therapy, while type 2 diabetes can sometimes be managed through lifestyle changes or oral medications.
- Understanding the distinctions between these two diabetes types is crucial for effective prevention and management.
- Ongoing research continues to explore potential cures and improved treatment options for both type 1 and type 2 diabetes.
Understanding Diabetes and Glucose Regulation
Glucose is a sugar that gives our bodies energy. We get it from food and it’s vital for many body functions. Keeping glucose levels right is key to health, especially for those with diabetes.
What is Glucose?
Glucose is a simple sugar that gets into our blood after eating carbs. It’s the main energy source for our cells. Keeping glucose levels balanced is important for health and preventing diseases.
The Role of Insulin
Insulin, made by the pancreas, is key to managing glucose. When blood glucose goes up, the pancreas makes insulin. This insulin helps glucose get into cells for energy or storage. This keeps blood sugar levels healthy.
The Pancreas and Islet Cells
The pancreas makes insulin. Inside it, islet cells release insulin and other hormones that control glucose. If the pancreas can’t make enough insulin or if the body doesn’t respond well, diabetes can happen.
Keeping glucose levels right is vital for health and avoiding diabetes complications. Knowing how glucose and insulin work is key to managing diabetes.
“Proper glucose regulation is essential for maintaining overall health and preventing the development of various medical conditions.”
Similarities in Type 1 and Type 2 Diabetes
Type 1 and type 2 diabetes have different causes but share many symptoms and risks. It’s important to know these similarities. This helps people spot diabetes signs early and get medical help fast.
Common Symptoms
People with both types of diabetes often have similar symptoms:
- Increased thirst and frequent urination
- Fatigue and lethargy
- Blurred vision
- Slow wound healing
Dangers of Uncontrolled Blood Sugar Levels
High blood sugar levels are a big problem for both types of diabetes. They can cause serious health issues, including:
- Damage to blood vessels, which raises the risk of heart disease, stroke, and peripheral artery disease
- Kidney damage, which could lead to kidney failure
- Nerve damage, causing neuropathy and foot problems
- Vision problems and blindness from diabetic retinopathy
It’s key for people with diabetes to know these symptoms and risks. They should get medical help quickly to manage their condition well.
Causes and Risk Factors: Type 1 Diabetes
Type 1 diabetes is an autoimmune disorder. It happens when the body’s immune system attacks and destroys insulin-producing cells in the pancreas. The exact cause is still a mystery, but it’s thought to be a mix of genetic factors and environmental triggers.
An Autoimmune Disorder
In type 1 diabetes, the body’s immune system makes antibodies that destroy the beta cells in the pancreas. These cells are key for making insulin. This process is believed to start with a mix of genetic predisposition and environmental factors, like viral infections.
Genetic and Environmental Factors
Having a family history of type 1 diabetes increases your risk. If a parent or sibling has it, you’re more likely to get it too. There are also age peaks for when the disease starts, with a big peak in kids aged four to seven and another in kids aged 10 to 14.
Environmental factors, like viral infections, also play a role. Some viruses might start the autoimmune response that destroys insulin-producing cells. But how these factors lead to type 1 diabetes is still a mystery.
| Key Factors in Type 1 Diabetes | Description |
|---|---|
| Autoimmune Disorder | The immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. |
| Genetic Factors | Family history and certain genetic predispositions can increase the risk of developing type 1 diabetes. |
| Environmental Factors | Viral infections and other environmental triggers may contribute to the development of the autoimmune response in type 1 diabetes. |
“The exact cause of type 1 diabetes is not fully understood, but it is believed to involve a combination of genetic and environmental factors that trigger an autoimmune response.”
Causes and Risk Factors: Type 2 Diabetes
Type 2 diabetes is mainly caused by insulin resistance. This is when the body’s cells don’t respond well to insulin. Lifestyle choices, like being overweight or not being active, play a big role. But, age, genetics, and ethnicity also have a part in it.
Insulin Resistance and Lifestyle Factors
Insulin resistance is a big reason for type 2 diabetes. When cells don’t take insulin well, they can’t use glucose right. This leads to high blood sugar. Being overweight, not moving much, and eating too much sugar or processed foods can make it worse.
Age, Genetics, and Ethnicity
Getting older, especially after 35, raises the risk of type 2 diabetes. If your family has it, you’re more likely to get it too. Some groups, like African Americans and Hispanics/Latinos, face a higher risk than others.
| Risk Factor | Description |
|---|---|
| Insulin Resistance | The body’s cells become less responsive to insulin, leading to elevated blood sugar levels. |
| Lifestyle Factors | Being overweight or obese, leading a sedentary lifestyle, and consuming a diet high in processed and sugary foods. |
| Age | The risk of type 2 diabetes increases with age, especially after the age of 35. |
| Genetics | Having a parent or sibling with type 2 diabetes increases the likelihood of developing the condition. |
| Ethnicity | Certain ethnic groups, such as African Americans, Hispanics/Latinos, American Indians, and Pacific Islanders, are at a higher risk of type 2 diabetes. |
Knowing what causes type 2 diabetes helps people take care of their health. They can lower their risk of getting this serious disease.
Diagnosis and Management of Type 1 Diabetes
People with type 1 diabetes need insulin because their bodies can’t make it. They must check their blood sugar often and adjust their insulin and diet. This helps them manage their diabetes well.
Insulin Therapy and Monitoring
Insulin therapy is the main treatment for type 1 diabetes. People with this condition need to take insulin shots or use an insulin pump. Checking their blood sugar regularly is key to keeping it balanced.
Dietary Considerations
Eating the right foods is important for managing type 1 diabetes. Counting carbs, controlling portions, and eating nutrient-rich foods helps keep blood sugar stable. A dietitian can help create a personalized diet plan.
Managing type 1 diabetes well involves insulin therapy, blood glucose monitoring, and the right diet. With the help of their healthcare team, people with type 1 diabetes can control their condition. This reduces the chance of serious problems later on.
“The main measurement for appropriate treatment of type 1 diabetes is the percentage of time spent daily with glucose levels between 70 and 180 milligrams per deciliter, which should be 70% or higher daily.”
Diagnosis and Management of Type 2 Diabetes
Managing type 2 diabetes often needs a mix of lifestyle changes and medical help. The first step is a proper diagnosis. This usually involves blood tests to check glucose levels.
Lifestyle Modifications
For those with type 2 diabetes, making lasting lifestyle changes is key. Eating healthy, exercising regularly, and keeping a healthy weight are important. Even a small weight loss of 5% can greatly improve health.
- Eat a balanced diet rich in whole, unprocessed foods
- Do at least 30 minutes of moderate exercise most days
- Add strength training to build muscle and boost metabolism
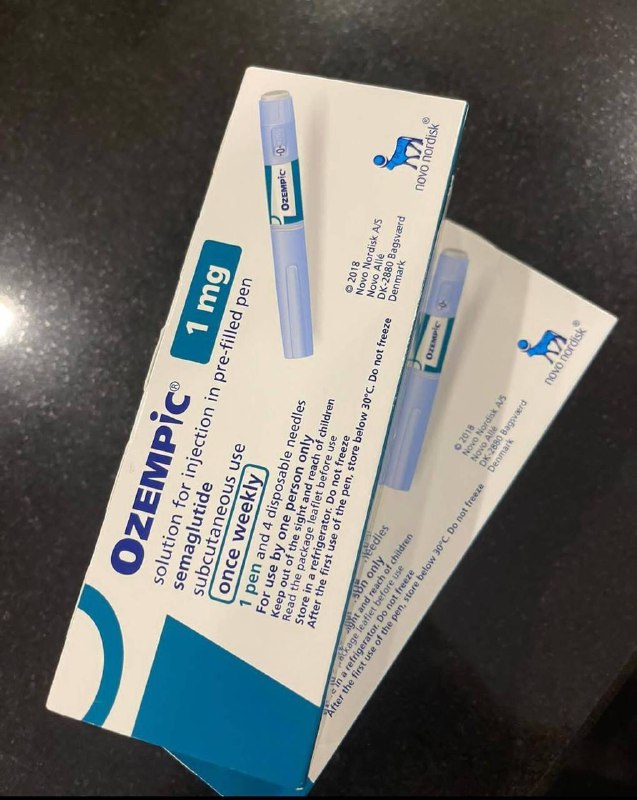
Medications and Insulin Therapy
Many with type 2 diabetes also need medication. Common diabetes medications include metformin, sulfonylureas, DPP-4 inhibitors, and GLP-1 agonists. Sometimes, insulin therapy is needed if insulin production or use is low.
| Medication | Mechanism of Action | Potential Side Effects |
|---|---|---|
| Metformin | Reduces hepatic glucose production and increases peripheral glucose uptake | Gastrointestinal issues, lactic acidosis |
| Sulfonylureas | Stimulate insulin secretion from pancreatic beta cells | Hypoglycemia, weight gain |
| DPP-4 Inhibitors | Inhibit the enzyme DPP-4, leading to increased insulin secretion | Urinary tract infections, pancreatitis |
| GLP-1 Agonists | Mimic the action of the GLP-1 hormone, which stimulates insulin secretion | Nausea, vomiting, diarrhea |
Keeping an eye on blood glucose levels and working closely with healthcare providers is vital. A comprehensive approach helps individuals manage their type 2 diabetes and improve their health.
type 1 v type 2 diabetes: Prevention Strategies
There’s no known way to stop type 1 diabetes from happening. But, you can delay or prevent type 2 diabetes with lifestyle changes and managing your weight.
Type 1 Diabetes: No Known Prevention
Type 1 diabetes is caused by the body attacking itself. Scientists still don’t know how to stop it. It usually starts in kids or teens. Managing it means taking insulin and checking blood sugar often.
Type 2 Diabetes: Lifestyle and Weight Management
Type 2 diabetes is different. It can be influenced by your lifestyle and health. Here are ways to prevent or delay type 2 diabetes:
- Keep a healthy weight: Losing 7-10% of your body weight can lower your risk by nearly 60%.
- Stay active: Do at least 150 minutes of moderate exercise a week. Also, do 2-3 strength training sessions to stay strong.
- Eat a fiber-rich diet: Eat lots of fruits, veggies, whole grains, and healthy fats. This helps with weight and health.
If you have prediabetes or are at risk for type 2 diabetes, talk to your doctor. They can help you make a plan to prevent it.
“Preventing type 2 diabetes is possible, and even a modest amount of weight loss can make a significant difference in reducing your risk.”
Emotional Impact of Diabetes
Living with diabetes, whether type 1 or type 2, can deeply affect a person’s emotions. Managing diabetes means always watching blood sugar levels and taking treatments. This can cause stress and anxiety. The stigma and wrong beliefs about diabetes also add to the emotional weight.
Coping with a Chronic Condition
People with diabetes face a big challenge in managing their condition. The stress of keeping blood sugar levels right, changing diets, and dealing with healthcare can hurt their mental health. A study by Goldney et al. in 2004 found a strong link between diabetes, depression, and quality of life.
- A meta-analytic review by Lustman et al. in 2000 showed that up to 30% of people with diabetes have depression.
- Katon et al.’s 2005 study found that having both depression and diabetes can increase death rates.
- An Indian study by Sridhar in 2007 found many people with diabetes also have mental health issues.
Stigma and Misconceptions
The stigma and wrong beliefs about diabetes make things worse emotionally. Many think diabetes is just because of bad choices, leading to judgment and misunderstanding.
“Diabetes is not just a physical condition; it has a significant emotional component as well. The stigma and misconceptions surrounding the disease can make it even more challenging for individuals to cope and manage their health effectively.”
To help with the emotional side of diabetes, healthcare and communities need to work together. They should offer mental health support and education to fight stigma. A caring and understanding environment helps people with diabetes face their challenges and improve their well-being.
Prevalence and Risk Factors by Demographics
Diabetes affects people of all ages, genders, and ethnicities. The prevalence and risk factors vary a lot. It’s key to understand these patterns to fight the diabetes epidemic and create better prevention and management plans.
Age, Gender, and Ethnicity
Type 1 diabetes often hits children and teens, while type 2 diabetes is more common in older folks. Worldwide, diabetes cases are expected to jump from 415 million in 2015 to 642 million by 2040. The elderly will see the highest rates.
In the US, more men (12.6%) have diabetes than women (10.8%). African Americans, Hispanic/Latino Americans, and American Indians face higher diabetes rates. This is due to socioeconomic and structural factors that lead to health disparities.
Health Disparities and Structural Inequities
The diabetes burden isn’t spread evenly. Socioeconomic status, healthcare access, and environment are key in diabetes development and management. People from disadvantaged communities often have higher diabetes rates, worse outcomes, and less access to quality care.
| Demographic Factors | Diabetes Prevalence |
|---|---|
| Age |
|
| Gender |
|
| Ethnicity |
|
“Addressing the disparities in diabetes prevalence and outcomes requires a comprehensive approach that tackles the underlying social, economic, and environmental factors driving these health inequities.”
Ongoing Research and Future Directions
The quest for a cure and better treatments for diabetes is a global effort. Scientists are studying the autoimmune causes of type 1 diabetes. They aim to find new ways to prevent or reverse it. Studies also focus on improving treatments for both types of diabetes to enhance quality of life.
Autoimmune Mechanisms and Potential Cures
Research has made big strides in understanding type 1 diabetes. A study by the American Diabetes Association found Hybrid Insulin Peptides as early detection markers. Another study showed that teplizumab can delay type 1 diabetes by up to 32.5 months, leading to FDA approval.
Stem cell research is also promising for type 1 diabetes treatment. It could replace lost insulin-producing cells. Scientists are working on using stem cells for new treatments.
Improving Treatments and Management Strategies
New medications like GLP1RAs, DPP-4 inhibitors, and SGLT-2 inhibitors have improved type 2 diabetes treatment. Researchers are also improving continuous glucose monitoring technology. They aim to make glucose sensors more stable and accurate.
Studies are looking into how obesity, hormones, and environmental factors affect diabetes. This knowledge is key to better management strategies and outcomes for people with diabetes.

The future of diabetes research is bright. By understanding autoimmune mechanisms, exploring cures, and improving treatments, scientists aim to better the lives of those with diabetes.
Conclusion
It’s important to know the differences between type 1 and type 2 diabetes. This knowledge helps those with diabetes, healthcare providers, and the public. By understanding the causes, risks, symptoms, and treatments for each type, we can improve care and outcomes.
People with type 2 diabetes face a higher risk of serious complications. These include kidney disease, eye problems, nerve damage, and high blood pressure. Early detection and lifestyle changes are key to reducing these risks.
Type 1 diabetes is caused by the body attacking its own insulin-making cells. It’s often linked to genetics. On the other hand, type 2 diabetes is often caused by lifestyle choices like not moving enough, eating poorly, and being overweight. Knowing these causes helps us find better ways to prevent and treat diabetes.